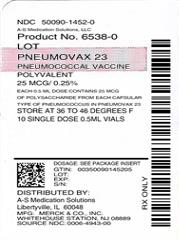
Label: PNEUMOVAX 23- pneumococcal vaccine polyvalent injection, solution
-
Contains inactivated NDC Code(s)
NDC Code(s): 50090-1452-0, 50090-1452-9 - Packager: A-S Medication Solutions
- This is a repackaged label.
- Source NDC Code(s): 0006-4943
- Category: VACCINE LABEL
- DEA Schedule: None
- Marketing Status: Biologic Licensing Application
Drug Label Information
Updated January 18, 2020
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PNEUMOVAX 23 safely and effectively. See full prescribing information for PNEUMOVAX 23.
PNEUMOVAX® 23 (pneumococcal vaccine polyvalent)
Sterile, Liquid Vaccine for Intramuscular or Subcutaneous
Injection
Initial U.S. Approval: 1983INDICATIONS AND USAGE
PNEUMOVAX 23 is a vaccine indicated for active immunization for the prevention of pneumococcal disease caused by the 23 serotypes contained in the vaccine (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F). (1.1)
PNEUMOVAX 23 is approved for use in persons 50 years of age or older and persons aged ≥2 years who are at increased risk for pneumococcal disease. (1.1, 14.1)
DOSAGE AND ADMINISTRATION
Single 0.5-mL dose of PNEUMOVAX 23 administered intramuscularly or subcutaneously only. (2.2)
DOSAGE FORMS AND STRENGTHS
Clear, sterile solution supplied in a (0.5-mL dose) single-dose vial and a single-dose, prefilled syringe. (3)
CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) to any component of PNEUMOVAX 23. (4.1)
WARNINGS AND PRECAUTIONS
- Use caution and appropriate care for individuals with severely compromised cardiovascular and/or pulmonary function in whom a systemic reaction would pose a significant risk. (5.2)
ADVERSE REACTIONS
The most common adverse reactions, reported in >10% of subjects vaccinated with PNEUMOVAX 23 in clinical trials, were: injection-site pain/soreness/tenderness (60.0%), injection-site swelling/induration (20.3%), headache (17.6%), injection-site erythema (16.4%), asthenia and fatigue (13.2%), and myalgia (11.9%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.
DRUG INTERACTIONS
In a randomized clinical study, a reduced immune response to ZOSTAVAX® as measured by gpELISA was observed in individuals who received concurrent administration of PNEUMOVAX 23 and ZOSTAVAX compared with individuals who received these vaccines 4 weeks apart. Consider administration of the two vaccines separated by at least 4 weeks. (7.1, 14.3)
USE IN SPECIFIC POPULATIONS
Pediatrics: PNEUMOVAX 23 is not approved for use in children younger than 2 years of age because children in this age group do not develop an effective immune response to capsular types contained in the polysaccharide vaccine. (8.4)
Geriatrics: For subjects aged 65 years or older in a clinical study systemic adverse reactions, determined by the investigator to be vaccine-related, were higher following revaccination (33.1%) than following initial vaccination (21.7%). Routine revaccination of immunocompetent persons previously vaccinated with a 23-valent vaccine, is not recommended. (8.5)
Immunocompromised Individuals: Response to vaccination may be diminished. (5.4, 8.6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 1/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Indications and Use
1.2 Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 Preparation
2.2 Administration
2.3 Revaccination
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
5 WARNINGS AND PRECAUTIONS
5.1 Persons with Moderate or Severe Acute Illness
5.2 Persons with Severely Compromised Cardiovascular or Pulmonary Function
5.3 Use of Antibiotic Prophylaxis
5.4 Persons with Altered Immunocompetence
5.5 Persons with Chronic Cerebrospinal Fluid Leakage
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
7 DRUG INTERACTIONS
7.1 Concomitant Administration with Other Vaccines
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Immunocompromised Individuals
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
14 CLINICAL STUDIES
14.1 Effectiveness
14.2 Immunogenicity
14.3 Concomitant Administration with Other Vaccines
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Indications and Use
PNEUMOVAX® 23 is a vaccine indicated for active immunization for the prevention of pneumococcal disease caused by the 23 serotypes contained in the vaccine (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F). PNEUMOVAX 23 is approved for use in persons 50 years of age or older and persons aged ≥2 years who are at increased risk for pneumococcal disease.
-
2 DOSAGE AND ADMINISTRATION
For intramuscular or subcutaneous injection only.
2.1 Preparation
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. If either of these two conditions exists, the vaccine should not be administered.
- Do not mix PNEUMOVAX 23 with other vaccines in the same syringe or vial.
- Use a separate sterile syringe and needle for each individual patient to prevent transmission of infectious agents from one person to another.
Single-Dose Vial
Withdraw 0.5 mL from the vial using a sterile needle and syringe free of preservatives, antiseptics, and detergents.
Single-Dose, Prefilled Syringe
The package does not contain a needle. Attach a sterile needle to the prefilled syringe by twisting in a clockwise direction until the needle fits securely on the syringe.
2.2 Administration
Administer PNEUMOVAX 23 intramuscularly or subcutaneously into the deltoid muscle or lateral mid-thigh. Do not inject intravascularly or intradermally.
2.3 Revaccination
The Advisory Committee on Immunization Practices (ACIP) has recommendations for revaccination against pneumococcal disease for persons at high risk who were previously vaccinated with PNEUMOVAX 23. Routine revaccination of immunocompetent persons previously vaccinated with a 23-valent vaccine, is not recommended.
-
3 DOSAGE FORMS AND STRENGTHS
PNEUMOVAX 23 is a clear, sterile solution supplied in a (0.5-mL dose) single-dose vial and a single-dose, prefilled syringe. [See Description (11) and How Supplied/Storage and Handling (16).]
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Do not administer PNEUMOVAX 23 to individuals with a history of anaphylactic/anaphylactoid or severe allergic reaction to any component of the vaccine. [See Description (11).]
-
5 WARNINGS AND PRECAUTIONS
5.1 Persons with Moderate or Severe Acute Illness
Defer vaccination with PNEUMOVAX 23 in persons with moderate or severe acute illness.
5.2 Persons with Severely Compromised Cardiovascular or Pulmonary Function
Caution and appropriate care should be exercised in administering PNEUMOVAX 23 to individuals with severely compromised cardiovascular and/or pulmonary function in whom a systemic reaction would pose a significant risk.
5.3 Use of Antibiotic Prophylaxis
This vaccine does not replace the need for penicillin (or other antibiotic) prophylaxis against pneumococcal infection. In patients who require penicillin (or other antibiotic) prophylaxis against pneumococcal infection, such prophylaxis should not be discontinued after vaccination with PNEUMOVAX 23.
5.4 Persons with Altered Immunocompetence
Persons who are immunocompromised, including persons receiving immunosuppressive therapy, may have a diminished immune response to PNEUMOVAX 23. [See Use in Specific Populations (8.6).]
-
6 ADVERSE REACTIONS
The most common adverse reactions, reported in >10% of subjects vaccinated with PNEUMOVAX 23 in clinical trials were: injection-site pain/soreness/tenderness (60.0%), injection-site swelling/induration (20.3%), headache (17.6%), injection-site erythema (16.4%), asthenia/fatigue (13.2%), and myalgia (11.9%). [See Adverse Reactions (6.1).]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
In a randomized, double-blind, placebo-controlled crossover clinical trial, subjects were enrolled in four different cohorts defined by age (50-64 years of age and ≥65 years of age) and vaccination status (no pneumococcal vaccination or receipt of a pneumococcal polysaccharide vaccine 3-5 years prior to the study). Subjects in each cohort were randomized to receive intramuscular injections of PNEUMOVAX 23 followed by placebo (saline containing 0.25% phenol), or placebo followed by PNEUMOVAX 23, at 30-day (±7 days) intervals. The safety of an initial vaccination (first dose) was compared to revaccination (second dose) with PNEUMOVAX 23 for 14 days following each vaccination.
All 1008 subjects (average age, 67 years; 49% male and 51% female; 91% Caucasian, 4.7% African-American, 3.5% Hispanic, and 0.8% Other) received placebo injections.
Initial vaccination was evaluated in a total of 444 subjects (average age 65 years; 32% male and 68% female; 93% Caucasian, 3.2% African-American, 3.4% Hispanic, and 1.1% Other).
Revaccination was evaluated in 564 subjects (average age 69 years; 53% male and 47% female; 90% Caucasian, 3.5% Hispanic, 6.0% African-American, and 0.5% Other).
Serious Adverse Experiences
In this study, 10 subjects had serious adverse experiences within 14 days of vaccination: 6 who received PNEUMOVAX 23 and 4 who received placebo. Serious adverse experiences within 14 days after PNEUMOVAX 23 included angina pectoris, heart failure, chest pain, ulcerative colitis, depression, and headache/tremor/stiffness/sweating. Serious adverse experiences within 14 days after placebo included myocardial infarction complicated with heart failure, alcohol intoxication, angina pectoris, and edema/urinary retention/heart failure/diabetes.
Five subjects reported serious adverse experiences that occurred outside the 14-day follow-up window: 3 who received PNEUMOVAX 23 and 2 who received placebo. Serious adverse experiences after PNEUMOVAX 23 included cerebrovascular accident, lumbar radiculopathy, and pancreatitis/myocardial infarction resulting in death. Serious adverse experiences after placebo included heart failure and motor vehicle accident resulting in death.
Solicited and Unsolicited Reactions
Table 1 presents the adverse event rates for all solicited and unsolicited reactions reported in ≥1% in any group in this study, without regard to causality.
The most common local adverse reactions reported at the injection site after initial vaccination with PNEUMOVAX 23 were pain/tenderness/soreness (60.0%), swelling/induration (20.3%), and erythema (16.4%). The most common systemic adverse experiences were headache (17.6%), asthenia/fatigue (13.2%), and myalgia (11.9%).
The most common local adverse reactions reported at the injection site after revaccination with PNEUMOVAX 23 were pain/soreness/tenderness (77.2%), swelling (39.8%), and erythema (34.5%). The most common systemic adverse reactions with revaccination were headache (18.1%), asthenia/fatigue (17.9%), and myalgia (17.3%). All of these adverse reactions were reported at a rate lower than 10% after receiving a placebo injection.
Table 1: Incidence of Injection-Site and Systemic Complaints in Adults ≥50 Years of Age Receiving Their First (Initial) or Second (Revaccination) Dose of PNEUMOVAX 23 (Pneumococcal Polysaccharide Vaccine, 23 Valent) or Placebo Occurring at ≥1% in Any Group PNEUMOVAX 23
Initial VaccinationPNEUMOVAX 23
Revaccination*Placebo Injection† N=444 N=564 N=1008 - *
- Subjects receiving their second dose of pneumococcal polysaccharide vaccine as PNEUMOVAX 23 approximately 3-5 years after their first dose.
- †
- Subjects receiving placebo injection from this study combined over periods.
- ‡
- The number of subjects receiving placebo followed for injection-site complaints. The corresponding number of subjects followed for systemic complaints was 981.
- §
- Fever events include subjects who felt feverish in addition to subjects with elevated temperature.
Number Followed for Safety 438 548 984‡ AE Rate AE Rate AE Rate Injection-Site Complaints Solicited Events Pain/Soreness/Tenderness 60.0% 77.2% 7.7% Swelling/Induration 20.3% 39.8% 2.8% Erythema 16.4% 34.5% 3.3% Unsolicited Events Ecchymosis 0% 1.1% 0.3% Pruritus 0.2% 1.6% 0.0% Systemic Complaints Solicited Events Asthenia/Fatigue 13.2% 17.9% 6.7% Chills 2.7% 7.8% 1.8% Myalgia 11.9% 17.3% 3.3% Headache 17.6% 18.1% 8.9% Unsolicited Events Fever§ 1.4% 2.0% 0.7% Diarrhea 1.1% 0.7% 0.5% Dyspepsia 1.1% 1.1% 0.9% Nausea 1.8% 1.8% 0.9% Back Pain 0.9% 0.9% 1.0% Neck Pain 0.7% 1.5% 0.2% Upper Respiratory
Infection1.8% 2.6% 1.8% Pharyngitis 1.1% 0.4% 1.3% In this clinical study an increased rate of local reactions was observed with revaccination at 3-5 years following initial vaccination.
For subjects aged 65 years or older, injection-site adverse reaction rate was higher following revaccination (79.3%) than following initial vaccination (52.9%). The proportion of subjects reporting injection site discomfort that interfered with or prevented usual activity or injection site induration ≥4 inches was higher following revaccination (30.6%) than following initial vaccination (10.4%). Injection site reactions typically resolved by 5 days following vaccination.
For subjects aged 50-64 years, the injection-site adverse reaction rate for revaccinees and initial vaccinees was similar (79.6% and 72.8% respectively).
The rate of systemic adverse reactions was similar among both initial vaccinees and revaccinees within each age group. The rate of vaccine-related systemic adverse reactions was higher following revaccination (33.1%) than following initial vaccination (21.7%) in subjects 65 years of age or older, and was similar following revaccination (37.5%) and initial vaccination (35.5%) in subjects 50-64 years of age. The most common systemic adverse reactions reported after PNEUMOVAX 23 were as follows: asthenia/fatigue, myalgia and headache.
Regardless of age, the observed increase in post vaccination use of analgesics (≤13% in the revaccinees and ≤4% in the initial vaccinees) returned to baseline by day 5.
6.2 Post-Marketing Experience
The following list of adverse reactions includes those identified during post approval use of PNEUMOVAX 23. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or their causal relationship to product exposure.
General disorders and administration site conditions
Cellulitis
Malaise
Fever (>102°F)
Warmth at the injection site
Decreased limb mobility
Peripheral edema in the injected extremityDigestive System
Nausea
VomitingHematologic/Lymphatic
Lymphadenitis
Lymphadenopathy
Thrombocytopenia in patients with stabilized idiopathic thrombocytopenic purpura
Hemolytic anemia in patients who have had other hematologic disorders
LeukocytosisHypersensitivity reactions including
Anaphylactoid reactions
Serum Sickness
Angioneurotic edemaMusculoskeletal System
Arthralgia
ArthritisNervous System
Paresthesia
Radiculoneuropathy
Guillain-Barré syndrome
Febrile convulsionSkin
Rash
Urticaria
Cellulitis-like reactions
Erythema multiformeInvestigations
Increased serum C-reactive protein -
7 DRUG INTERACTIONS
7.1 Concomitant Administration with Other Vaccines
In a randomized clinical study, a reduced immune response to ZOSTAVAX® as measured by gpELISA was observed in individuals who received concurrent administration of PNEUMOVAX 23 and ZOSTAVAX compared with individuals who received these vaccines 4 weeks apart. Consider administration of the two vaccines separated by at least 4 weeks. [See Clinical Studies (14.3).]
Limited safety and immunogenicity data from clinical trials are available on the concurrent administration of PNEUMOVAX 23 and vaccines other than ZOSTAVAX.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Available human data from clinical trials of PNEUMOVAX 23 in pregnancy have not established the presence or absence of a vaccine-associated risk.
Developmental toxicity studies have not been conducted with PNEUMOVAX 23 in animals.
8.2 Lactation
Risk Summary
It is not known whether PNEUMOVAX 23 is excreted in human milk. Data are not available to assess the effects of PNEUMOVAX 23 on the breastfed infant or on milk production/excretion.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for PNEUMOVAX 23 and any potential adverse effects on the breastfed child from PNEUMOVAX 23 or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to the disease prevented by the vaccine.
8.4 Pediatric Use
PNEUMOVAX 23 is not approved for use in children less than 2 years of age. Children in this age group do not develop an effective immune response to the capsular types contained in this polysaccharide vaccine.
The ACIP has recommendations for use of PNEUMOVAX 23 in children 2 years of age or older, who have previously received pneumococcal vaccines, and who are at increased risk for pneumococcal disease.
8.5 Geriatric Use
In one clinical trial of PNEUMOVAX 23, conducted post-licensure, a total of 629 subjects who were aged ≥65 years and 201 subjects who were aged ≥75 years were enrolled.
In this trial, the safety of PNEUMOVAX 23 in adults 65 years of age and older (N=629) was compared to the safety of PNEUMOVAX 23 in adults 50 to 64 years of age (N=379). The subjects in this study had underlying chronic illness but were in stable condition; at least 1 medical condition at enrollment was reported by 86.3% of subjects who were 50 to 64 years old, and by 96.7% of subjects who were 65 to 91 years old. The rate of vaccine-related systemic adverse experiences was higher following revaccination (33.1%) than following primary vaccination (21.7%) in subjects ≥65 years of age, and was similar following revaccination (37.5%) and primary vaccination (35.5%) in subjects 50 to 64 years of age.
Since elderly individuals may not tolerate medical interventions as well as younger individuals, a higher frequency and/or a greater severity of reactions in some older individuals cannot be ruled out.
Post-marketing reports have been received in which some elderly individuals had severe adverse experiences and a complicated clinical course following vaccination. Some individuals with underlying medical conditions of varying severity experienced local reactions and fever associated with clinical deterioration requiring hospital care.
-
11 DESCRIPTION
PNEUMOVAX 23 (Pneumococcal Vaccine Polyvalent) is a sterile, liquid vaccine consisting of a mixture of purified capsular polysaccharides from Streptococcus pneumoniae types (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F).
PNEUMOVAX 23 is a clear, colorless solution. Each 0.5-mL dose of vaccine contains 25 micrograms of each polysaccharide type in isotonic saline solution containing 0.25% phenol as a preservative. The vaccine is used directly as supplied. No dilution or reconstitution is necessary.
The vial stoppers, syringe plunger stopper and syringe tip cap are not made with natural rubber latex.
- 12 CLINICAL PHARMACOLOGY
-
14 CLINICAL STUDIES
14.1 Effectiveness
The protective efficacy of pneumococcal vaccines containing six (types 1, 2, 4, 8, 12F, and 25) or twelve (types 1, 2, 3, 4, 6A, 8, 9N, 12F, 25, 7F, 18C, and 46) capsular polysaccharides was investigated in two controlled studies in South Africa in male novice gold miners ranging in age from 16 to 58 years, in whom there was a high attack rate for pneumococcal pneumonia and bacteremia. In both studies, participants in the control groups received either meningococcal polysaccharide serogroup A vaccine or saline placebo. In both studies, attack rates for vaccine type pneumococcal pneumonia were observed for the period from 2 weeks through about 1 year after vaccination. Protective efficacy was 76% and 92%, respectively, for the 6- and 12-valent vaccines, for the capsular types represented.
Three similar studies in South African young adult male novice gold miners were carried out by Dr. R. Austrian and associates using similar pneumococcal vaccines prepared for the National Institute of Allergy and Infectious Diseases, with pneumococcal vaccines containing a 6-valent formulation (types 1, 3, 4, 7, 8, and 12) or a 13-valent formulation (types 1, 2, 3, 4, 6, 7, 8, 9, 12, 14, 18, 19, and 25) capsular polysaccharides. The reduction in pneumococcal pneumonia caused by the capsular types contained in the vaccines was 79%. Reduction in type-specific pneumococcal bacteremia was 82%.
A prospective study in France found a pneumococcal vaccine containing fourteen (types 1, 2, 3, 4, 6A, 7F, 8, 9N, 12F, 14, 18C, 19F, 23F, and 25) capsular polysaccharides to be 77% (95%CI: 51% to 89%) effective in reducing the incidence of pneumonia among male and female nursing home residents with a mean age of 74 (standard deviation of 4 years).
In a study using a pneumococcal vaccine containing eight (types 1, 3, 6, 7, 14, 18, 19, and 23) capsular polysaccharides, vaccinated children and young adults aged 2 to 25 years who had sickle cell disease, congenital asplenia, or undergone a splenectomy experienced significantly less bacteremic pneumococcal disease than patients who were not vaccinated.
In the United States, one post-licensure randomized controlled trial, in the elderly or patients with chronic medical conditions who received a 14-valent pneumococcal polysaccharide vaccine (types 1, 2, 3, 4, 6A, 8, 9N, 12F, 14, 19F, 23F, 25, 7F, and 18C), did not support the efficacy of the vaccine for nonbacteremic pneumonia.
A retrospective cohort analysis study based on the U.S. Centers for Disease Control and Prevention (CDC) pneumococcal surveillance system, showed 57% (95%CI: 45% to 66%) overall protective effectiveness against invasive infections caused by serotypes included in PNEUMOVAX 23 in persons ≥6 years of age, 65 to 84% effectiveness among specific patient groups (e.g., persons with diabetes mellitus, coronary vascular disease, congestive heart failure, chronic pulmonary disease, and anatomic asplenia) and 75% (95%CI: 57% to 85%) effectiveness in immunocompetent persons aged ≥65 years of age. Vaccine effectiveness could not be confirmed for certain groups of immunocompromised patients.
14.2 Immunogenicity
The levels of antibodies that correlate with protection against pneumococcal disease have not been clearly defined.
Antibody responses to most pneumococcal capsular types are generally low or inconsistent in children less than 2 years of age.
14.3 Concomitant Administration with Other Vaccines
In a double-blind, controlled clinical trial, 473 adults, 60 years of age or older, were randomized to receive ZOSTAVAX and PNEUMOVAX 23 concomitantly (N=237), or PNEUMOVAX 23 alone followed 4 weeks later by ZOSTAVAX alone (N=236). At four weeks postvaccination, the varicella-zoster virus (VZV) antibody levels following concomitant use were significantly lower than the VZV antibody levels following nonconcomitant administration (GMTs of 338 vs. 484 gpELISA units/mL, respectively; GMT ratio = 0.70 (95% CI: [0.61, 0.80]).
Limited safety and immunogenicity data from clinical trials are available on the concurrent administration of PNEUMOVAX 23 and vaccines other than ZOSTAVAX.
- 16 HOW SUPPLIED/STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Inform the patient, parent or guardian of the benefits and risks associated with vaccination.
- Tell the patient, parent or guardian that vaccination with PNEUMOVAX 23 may not offer 100% protection from pneumococcal infection.
- Provide the patient, parent or guardian with the vaccine information statements required by the National Childhood Vaccine Injury Act of 1986, with each immunization.
- Instruct the patient, parent or guardian to report any serious adverse reactions to their health care provider who in turn should report such events to the vaccine manufacturer or the U.S. Department of Health and Human Services through the Vaccine Adverse Event Reporting System (VAERS), 1-800-822-7967, or report online at www.vaers.hhs.gov.
-
SPL UNCLASSIFIED SECTION
Manuf. and Dist. by: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USAFor patent information: www.merck.com/product/patent/home.html
The trademarks depicted herein are owned by their respective companies.
Copyright © 1986-2019 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved.uspi-v110-i-1911r042
-
PATIENT PACKAGE INSERT
Patient Information about
PNEUMOVAX® 23 (pronounced "noo-mo-vax 23")
Generic Name: pneumococcal vaccine polyvalentRead this leaflet before you or your child gets the vaccine called PNEUMOVAX 23. If you have any questions about the vaccine after you read this, you should ask your health care provider. This is a summary only. It does not take the place of talking to your doctor, nurse or other health care provider about the vaccine. Only your health care provider can decide if PNEUMOVAX 23 is right for you or your child.
What is PNEUMOVAX 23?
PNEUMOVAX 23 is a vaccine that is given as a shot. It helps protect you from infection by certain germs or bacteria which are called pneumococcus (pronounced "noo-mo-ca-cus"). PNEUMOVAX 23 is for people 50 years of age and older. It is also for people who are 2 years of age and older if they have certain medical conditions that put them at increased risk for infection.
Illnesses or health problems may allow these germs to spread into the blood, lungs, or brain where they can cause serious diseases such as:
- An infection in the blood
- A lung infection (pneumonia) that can also come with an infection in the blood
- An infection of the coverings of the brain and spinal cord (meningitis).
PNEUMOVAX 23 may not protect everyone who gets it. It will not protect against diseases that are caused by bacteria types that are not in the vaccine.
Who should not get PNEUMOVAX 23?
You should not get this vaccine if you (or your child):
- are allergic to any of its ingredients
- had an allergic reaction to PNEUMOVAX 23 in the past
- are less than 2 years old.
What should I tell my health care provider before getting PNEUMOVAX 23?
Tell your health care provider if you (or your child):
- are allergic to PNEUMOVAX 23
- have heart or lung problems
- have a fever
- have immune problems or are receiving radiation treatment for chemotherapy
- are pregnant or breast-feeding
How is PNEUMOVAX 23 given?
Most often, just one shot is given.
If you or your child is in a high-risk group for pneumococcal infection, then your health care provider will decide if it would be helpful to give a second shot of PNEUMOVAX 23 at a later time.
Can PNEUMOVAX 23 be given with other vaccines?
Talk to your health care provider if you plan to get ZOSTAVAX at the same time as PNEUMOVAX 23 because it may be better to get these vaccines at least 4 weeks apart.
Talk to your health care provider if you plan to get PNEUMOVAX 23 at the same time as other vaccines.
What are the possible side effects of PNEUMOVAX 23?
The most common side effects are:
- pain, warmth, soreness, redness, swelling, and hardening at the injection site
- headache
- weakness, feeling tired
- muscle pain
Tell your health care provider or get emergency help right away if you get any of the following problems after vaccination because these may be signs of an allergic reaction or other serious conditions:
- difficulty breathing
- wheezing
- rash
- hives
Side effects at the site where you get the shot may be more common and may feel worse after a second shot than after the first shot.
Tell your health care provider if you or your child has a side effect that bothers you or that does not go away.
For a more complete list of side effects, ask your health care provider.
You may also report any side effect to your or your child's health care provider, or directly to the Vaccine Adverse Event Reporting System (VAERS). You may call the VAERS number 1-800-822-7967 at no charge, or report online to www.vaers.hhs.gov.
What are the ingredients of PNEUMOVAX 23?
Active Ingredients: Bacterial sugars from 23 pneumococcal types: 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F Inactive Ingredients: Phenol (a preservative) What else should I know about PNEUMOVAX 23?
Some adults and children have problems with leakage of spinal fluid after the skull is cracked or injured or after medical operations and this may increase their risk for pneumococcal infection. PNEUMOVAX 23 may not be able to prevent all of these infections.
The vial stoppers, syringe plunger stopper and syringe tip cap for PNEUMOVAX 23 are not made with natural rubber latex.
This leaflet is a summary of information about PNEUMOVAX 23. If you would like more information, talk to your health care provider. You can also call the Merck National Service Center at 1-800-622-4477.
-
SPL UNCLASSIFIED SECTION
Manuf. and Dist. by: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USAFor patent information: www.merck.com/product/patent/home.html
Copyright © 2011 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved.Revised: 05/2015
usppi-v110-i-1505r039
Printed in USA
Rx Only
- Storage
- pneumococcal vaccine polyvalent
-
INGREDIENTS AND APPEARANCE
PNEUMOVAX 23
pneumococcal vaccine polyvalent injection, solutionProduct Information Product Type VACCINE Item Code (Source) NDC:50090-1452(NDC:0006-4943) Route of Administration INTRAMUSCULAR, SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: H9NOI61UH1) (STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:H9NOI61UH1) STREPTOCOCCUS PNEUMONIAE TYPE 1 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 2 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: E11P4F3X4S) (STREPTOCOCCUS PNEUMONIAE TYPE 2 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:E11P4F3X4S) STREPTOCOCCUS PNEUMONIAE TYPE 2 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 4FVB62AFF1) (STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:4FVB62AFF1) STREPTOCOCCUS PNEUMONIAE TYPE 3 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: CGS5KI3Q2M) (STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:CGS5KI3Q2M) STREPTOCOCCUS PNEUMONIAE TYPE 4 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: N8R9GL539D) (STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:N8R9GL539D) STREPTOCOCCUS PNEUMONIAE TYPE 5 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 57F7254B6Q) (STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:57F7254B6Q) STREPTOCOCCUS PNEUMONIAE TYPE 6B CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: X1K54R2P9I) (STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:X1K54R2P9I) STREPTOCOCCUS PNEUMONIAE TYPE 7F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 669818346F) (STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:669818346F) STREPTOCOCCUS PNEUMONIAE TYPE 8 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 9N CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 313LJP87ET) (STREPTOCOCCUS PNEUMONIAE TYPE 9N CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:313LJP87ET) STREPTOCOCCUS PNEUMONIAE TYPE 9N CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: DL82PE6ANE) (STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:DL82PE6ANE) STREPTOCOCCUS PNEUMONIAE TYPE 9V CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 328VNB72T8) (STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:328VNB72T8) STREPTOCOCCUS PNEUMONIAE TYPE 10A CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: N967BGT6XW) (STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:N967BGT6XW) STREPTOCOCCUS PNEUMONIAE TYPE 11A CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: S46U1CM432) (STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:S46U1CM432) STREPTOCOCCUS PNEUMONIAE TYPE 12F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: G1GFK9898U) (STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:G1GFK9898U) STREPTOCOCCUS PNEUMONIAE TYPE 14 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 667Y1EG6EW) (STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:667Y1EG6EW) STREPTOCOCCUS PNEUMONIAE TYPE 15B CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 17F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 3RED79E75R) (STREPTOCOCCUS PNEUMONIAE TYPE 17F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:3RED79E75R) STREPTOCOCCUS PNEUMONIAE TYPE 17F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 23036553F6) (STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:23036553F6) STREPTOCOCCUS PNEUMONIAE TYPE 18C CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 5K0VU709JD) (STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:5K0VU709JD) STREPTOCOCCUS PNEUMONIAE TYPE 19F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 9W2T4OSF98) (STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:9W2T4OSF98) STREPTOCOCCUS PNEUMONIAE TYPE 19A CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 20 CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: V3FC0DK9XS) (STREPTOCOCCUS PNEUMONIAE TYPE 20 CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:V3FC0DK9XS) STREPTOCOCCUS PNEUMONIAE TYPE 20 CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 7NLV25LOSI) (STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:7NLV25LOSI) STREPTOCOCCUS PNEUMONIAE TYPE 22F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: PYD255827T) (STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:PYD255827T) STREPTOCOCCUS PNEUMONIAE TYPE 23F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE ANTIGEN (UNII: 2MGG3XW1L2) (STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE ANTIGEN - UNII:2MGG3XW1L2) STREPTOCOCCUS PNEUMONIAE TYPE 33F CAPSULAR POLYSACCHARIDE ANTIGEN 25 ug in 0.5 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:50090-1452-0 10 in 1 CARTON 1 NDC:50090-1452-9 .5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA101094 07/07/1983 Labeler - A-S Medication Solutions (830016429) Establishment Name Address ID/FEI Business Operations A-S Medication Solutions 830016429 RELABEL(50090-1452)