Label: CYCLOSPORINE capsule, gelatin coated
- NDC Code(s): 68084-879-25, 68084-879-95, 68084-921-25, 68084-921-95
- Packager: American Health Packaging
- This is a repackaged label.
- Source NDC Code(s): 60505-0133, 60505-0134
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated May 13, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
BOXED WARNING
(What is this?)
WARNING
Only physicians experienced in immunosuppressive therapy and management of organ transplant patients should prescribe cyclosporine capsules, (NON-MODIFIED). Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
Cyclosporine capsules, (NON-MODIFIED) should be administered with adrenal corticosteroids but not with other immunosuppressive agents. Increased susceptibility to infection and the possible development of lymphoma may result from immunosuppression.
Cyclosporine capsules, (NON-MODIFIED) have decreased bioavailability in comparison to Neoral ®* (cyclosporine capsules, USP) MODIFIED.
Cyclosporine capsules, (NON-MODIFIED) and Neoral ®* (cyclosporine capsules, USP) MODIFIED are not bioequivalent and cannot be used interchangeably without physician supervision.
The absorption of cyclosporine during chronic administration of cyclosporine capsules, (NON-MODIFIED) was found to be erratic. It is recommended that patients taking cyclosporine capsules, (NON-MODIFIED) over a period of time be monitored at repeated intervals for cyclosporine blood concentrations and subsequent dose adjustments be made in order to avoid toxicity due to high concentrations and possible organ rejection due to low absorption of cyclosporine. This is of special importance in liver transplants. Numerous assays are being developed to measure blood concentrations of cyclosporine. Comparison of concentrations in published literature to patient concentrations using current assays must be done with detailed knowledge of the assay methods employed. (SeeDOSAGE AND ADMINISTRATION, Blood Concentration Monitoring.)
-
DESCRIPTION
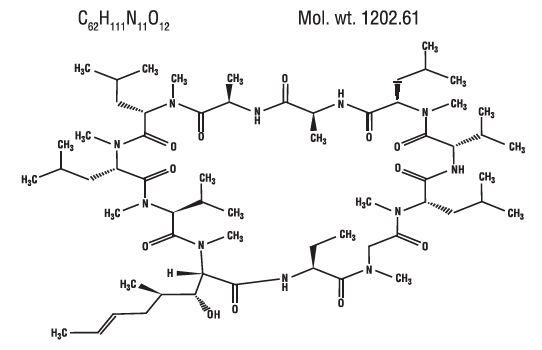
Cyclosporine, USP, the active principle in cyclosporine capsules, USP (NON-MODIFIED) is a cyclic polypeptide immunosuppressant agent consisting of 11 amino acids. It is produced as a metabolite by the fungus species Tolypocladium inflatum Gams.
Chemically, cyclosporine is designated as [ R-[ R*, R*-( E)]]-cyclic(L-alanyl-D-alanyl- N-methyl-L-leucyl- N-methyl-L-leucyl- N-methyl-L-valyl-3-hydroxy- N,4-dimethyl-L-2-amino-6-octenoyl-L-α-amino-butyryl- N-methylglycyl- N-methyl-L-leucyl-L-valyl- N-methyl-L-leucyl).
Cyclosporine capsules, USP (NON-MODIFIED) are available in 25 mg and 100 mg strengths.
Each 25 mg capsule contains:
Cyclosporine, USP……………………………………………………………………...25 mgEach 100 mg capsule contains:
Cyclosporine, USP……………………………………………………..……………...100 mgEach capsule contains the following inactive ingredients: methanol, sodium lauryl sulfate and talc. The 25 mg and the 100 mg capsule shell contains gelatin, red iron oxide and titanium dioxide.
The 25 mg and 100 mg capsule black imprinting ink contains the following inactive ingredients: n-butyl alcohol, D&C yellow #10 aluminum lake, FD&C blue #1 aluminum lake, FD&C blue #2 aluminum lake, FD&C red #40 aluminum lake, pharmaceutical glaze, propylene glycol, SDA-3A alcohol and synthetic black iron oxide.
The chemical structure of cyclosporine (also known as cyclosporin A) is:
-
CLINICAL PHARMACOLOGY
Cyclosporine is a potent immunosuppressive agent, which in animals prolongs survival of allogeneic transplants involving skin, heart, kidney, pancreas, bone marrow, small intestine, and lung. Cyclosporine has been demonstrated to suppress some humoral immunity and to a greater extent, cell-mediated reactions, such as allograft rejection, delayed hypersensitivity, experimental allergic encephalomyelitis, Freund's adjuvant arthritis, and graft vs. host disease in many animal species for a variety of organs.
Successful kidney, liver, and heart allogeneic transplants have been performed in man using cyclosporine.
The exact mechanism of action of cyclosporine is not known. Experimental evidence suggests that the effectiveness of cyclosporine is due to specific and reversible inhibition of immunocompetent lymphocytes in the G 0- or G 1-phase of the cell cycle. T-lymphocytes are preferentially inhibited. The T-helper cell is the main target, although the T-suppressor cell may also be suppressed. Cyclosporine also inhibits lymphokine production and release, including interleukin-2 or T-cell growth factor (TCGF).
No functional effects on phagocytic (changes in enzyme secretions not altered, chemotactic migration of granulocytes, macrophage migration, carbon clearance in vivo) or tumor cells (growth rate, metastasis) can be detected in animals. Cyclosporine does not cause bone marrow suppression in animal models or man.
The absorption of cyclosporine from the gastrointestinal tract is incomplete and variable. Peak concentrations (C max) in blood and plasma are achieved at about 3.5 hours. C max and area under the plasma or blood concentration/time curve (AUC) increase with the administered dose; for blood, the relationship is curvilinear (parabolic) between 0 and 1400 mg. As determined by a specific assay, C max is approximately 1 ng/mL/mg of dose for plasma and 2.7 to 1.4 ng/mL/mg of dose for blood (for low to high doses).
Cyclosporine is distributed largely outside the blood volume. In blood, the distribution is concentration dependent. Approximately 33% to 47% is in plasma, 4% to 9% in lymphocytes, 5% to 12% in granulocytes, and 41% to 58% in erythrocytes. At high concentrations, the uptake by leukocytes and erythrocytes becomes saturated. In plasma, approximately 90% is bound to proteins, primarily lipoproteins.
The disposition of cyclosporine from blood is biphasic with a terminal half-life of approximately 19 hours (range, 10 to 27 hours). Elimination is primarily biliary with only 6% of the dose excreted in the urine.
Cyclosporine is extensively metabolized but there is no major metabolic pathway. Only 0.1% of the dose is excreted in the urine as unchanged drug. Of 15 metabolites characterized in human urine, 9 have been assigned structures. The major pathways consist of hydroxylation of the Cγ-carbon of 2 of the leucine residues, Cη-carbon hydroxylation, and cyclic ether formation (with oxidation of the double bond) in the side chain of the amino acid 3-hydroxyl- N,4-dimethyl-L-2-amino-6-octenoic acid and N-demethylation of N-methyl leucine residues. Hydrolysis of the cyclic peptide chain or conjugation of the aforementioned metabolites do not appear to be important biotransformation pathways.
Specific Populations
Renal Impairment
In a study performed in 4 subjects with end-stage renal disease (creatinine clearance <5 mL/min), an intravenous infusion of 3.5 mg/kg of cyclosporine over 4 hours administered at the end of a hemodialysis session resulted in a mean volume of distribution (Vdss) of 3.49 L/kg and systemic clearance (CL) of 0.369 L/hr/kg. This systemic CL (0.369 L/hr/kg) was approximately two thirds of the mean systemic CL (0.56 L/hr/kg) of cyclosporine in historical control subjects with normal renal function. In 5 liver transplant patients, the mean clearance of cyclosporine on and off hemodialysis was 463 mL/min and 398 mL/min, respectively. Less than 1% of the dose of cyclosporine was recovered in the dialysate.Hepatic Impairment
Cyclosporine is extensively metabolized by the liver. Since severe hepatic impairment may result in significantly increased cyclosporine exposures, the dosage of cyclosporine may need to be reduced in these patients. -
INDICATIONS AND USAGE
Cyclosporine capsules, (NON-MODIFIED) are indicated for the prophylaxis of organ rejection in kidney, liver, and heart allogeneic transplants. It is always to be used with adrenal corticosteroids. The drug may also be used in the treatment of chronic rejection in patients previously treated with other immunosuppressive agents.
- CONTRAINDICATIONS
-
WARNINGS
Kidney, Liver, and Heart Transplant
Cyclosporine capsules, (NON-MODIFIED), when used in high doses, can cause hepatotoxicity and nephrotoxicity (see Boxed Warning.)Nephrotoxicity
It is not unusual for serum creatinine and BUN levels to be elevated during cyclosporine therapy. These elevations in renal transplant patients do not necessarily indicate rejection, and each patient must be fully evaluated before dosage adjustment is initiated.Nephrotoxicity has been noted in 25% of cases of renal transplantation, 38% of cases of cardiac transplantation, and 37% of cases of liver transplantation. Mild nephrotoxicity was generally noted 2 to 3 months after transplant and consisted of an arrest in the fall of the preoperative elevations of BUN and creatinine at a range of 35 to 45 mg/dl and 2.0 to 2.5 mg/dl, respectively. These elevations were often responsive to dosage reduction.
More overt nephrotoxicity was seen early after transplantation and was characterized by a rapidly rising BUN and creatinine. Since these events are similar to rejection episodes, care must be taken to differentiate between them. This form of nephrotoxicity is usually responsive to cyclosporine capsules dosage reduction.
Although specific diagnostic criteria which reliably differentiate renal graft rejection from drug toxicity have not been found, a number of parameters have been significantly associated to one or the other. It should be noted however, that up to 20% of patients may have simultaneous nephrotoxicity and rejection.
Nephrotoxicity vs. Rejection
Parameter
Nephrotoxicity
Rejection
History
Donor > 50 years old or hypotensive
Antidonor immune response
Prolonged kidney preservation
Prolonged anastomosis time
Retransplant patient
Concomitant nephrotoxic drugs
Clinical
Often > 6 weeks postop *
Often < 4 weeks postop †
Prolonged initial nonfunction
Fever > 37.5°C
(acute tubular necrosis)
Weight gain > 0.5 kg
Graft swelling and tenderness
Decrease in daily urine volume > 500 mL (or 50%)
Laboratory
CyA serum trough level > 200 ng/mL
CyA serum trough level < 150 ng/mL
Gradual rise in Cr (< 0.15 mg/dL/day) *
Rapid rise in Cr (> 0.3 mg/dL/day) *
Cr plateau < 25% above baseline
Cr > 25% above baseline
BUN/Cr ≥ 20
BUN/Cr < 20
Biopsy
Arteriolopathy (medial hypertrophy *,
hyalinosis, nodular deposits, intimal
intimal arteritis †, necrosis, sclerosis)
thickening, endothelial vacuolization,
progressive scarring)
Tubular atrophy, isometric vacuolization,
isolated calcifications
some irregular vacuolization
Minimal edema
Mild focal infiltrates ‡
Diffuse moderate to severe mononuclear
infiltrates §
Diffuse interstitial fibrosis, often striped form
Glomerulitis (mononuclear cells) ‡
Aspiration Cytology
CyA deposits in tubular and endothelial cells
Inflammatory infiltrate with mononuclear phagocytes, macrophages, lymphoblastoid cells, and activated T-cells
Fine isometric vacuolization of tubular cells
These strongly express HLA-DR antigens
Urine Cytology
Tubular cells with vacuolization and
Degenerative tubular cells, plasma cells, and
granularization
lymphocyturia > 20% of sediment
Manometry
Intracapsular pressure < 40 mm Hg †
Intracapsular pressure > 40 mm Hg †
Ultrasonography
Unchanged graft cross-sectional area
Increase in graft cross-sectional area
AP diameter ≥ Transverse diameter
Magnetic Resonance Imagery
Normal appearance
Loss of distinct corticomedullary junction, swelling, image intensity of parachyma approaching that of psoas, loss of hilar fat
Radionuclide Scan
Normal or generally decreased perfusion
Patchy arterial flow
Decrease in tubular function
Decrease in perfusion > decrease in tubular function
( 131I-hippuran) > decrease in perfusion
Increased uptake of Indium 111 labeled platelets or Tc-99m in colloid
( 99mTc DTPA)
Therapy
Responds to decreased cyclosporine capsules
Responds to increased steroids or antilymphocyte globulin
A form of chronic progressive cyclosporine-associated nephrotoxicity is characterized by serial deterioration in renal function and morphologic changes in the kidneys. From 5% to 15% of transplant recipients will fail to show a reduction in a rising serum creatinine despite a decrease or discontinuation of cyclosporine therapy. Renal biopsies from these patients will demonstrate an interstitial fibrosis with tubular atrophy. In addition, toxic tubulopathy, peritubular capillary congestion, arteriolopathy, and a striped form of interstitial fibrosis with tubular atrophy may be present. Though none of these morphologic changes is entirely specific, a histologic diagnosis of chronic progressive cyclosporine-associated nephrotoxicity requires evidence of these.
When considering the development of chronic nephrotoxicity it is noteworthy that several authors have reported an association between the appearance of interstitial fibrosis and higher cumulative doses or persistently high circulating trough concentrations of cyclosporine. This is particularly true during the first 6 posttransplant months when the dosage tends to be highest and when, in kidney recipients, the organ appears to be most vulnerable to the toxic effects of cyclosporine. Among other contributing factors to the development of interstitial fibrosis in these patients must be included, prolonged perfusion time, warm ischemia time, as well as episodes of acute toxicity, and acute and chronic rejection. The reversibility of interstitial fibrosis and its correlation to renal function have not yet been determined.
Impaired renal function at any time requires close monitoring, and frequent dosage adjustment may be indicated. In patients with persistent high elevations of BUN and creatinine who are unresponsive to dosage adjustments, consideration should be given to switching to other immunosuppressive therapy. In the event of severe and unremitting rejection, it is preferable to allow the kidney transplant to be rejected and removed rather than increase the cyclosporine capsules dosage to a very high level in an attempt to reverse the rejection.
Due to the potential for additive or synergistic impairment of renal function, caution should be exercised when coadministering cyclosporine capsules with other drugs that may impair renal function (see PRECAUTIONS, Drug Interactions).
Thrombotic Microangiopathy
Occasionally patients have developed a syndrome of thrombocytopenia and microangiopathic hemolytic anemia which may result in graft failure. The vasculopathy can occur in the absence of rejection and is accompanied by avid platelet consumption within the graft as demonstrated by Indium 111 labeled platelet studies. Neither the pathogenesis nor the management of this syndrome is clear. Though resolution has occurred after reduction or discontinuation of cyclosporine capsules and 1) administration of streptokinase and heparin or 2) plasmapheresis, this appears to depend upon early detection with Indium 111 labeled platelet scans (see ADVERSE REACTIONS).Hyperkalemia
Significant hyperkalemia (sometimes associated with hyperchloremic metabolic acidosis) and hyperuricemia have been seen occasionally in individual patients.Hepatotoxicity
Cases of hepatotoxicity and liver injury including cholestasis, jaundice, hepatitis, and liver failure have been reported in patients treated with cyclosporine. Most reports included patients with significant co-morbidities, underlying conditions and other confounding factors including infectious complications and comedications with hepatotoxic potential. In some cases, mainly in transplant patients, fatal outcomes have been reported (see ADVERSE REACTIONS, Postmarketing Experience).Hepatotoxicity, usually manifested by elevations in hepatic enzymes and bilirubin, was reported in patients treated with cyclosporine in clinical trials: 4% in renal transplantation, 7% in cardiac transplantation, and 4% in liver transplantation. This was usually noted during the first month of therapy when high doses of cyclosporine capsules were used. The chemistry elevations usually decreased with a reduction in dosage.
Malignancies
As in patients receiving other immunosuppressants, those patients receiving cyclosporine capsules are at increased risk for development of lymphomas and other malignancies, particularly those of the skin. The increased risk appears related to the intensity and duration of immunosuppression rather than to the use of specific agents. Because of the danger of oversuppression of the immune system, which can also increase susceptibility to infection, cyclosporine capsules should not be administered with other immunosuppressive agents except adrenal corticosteroids. The efficacy and safety of cyclosporine in combination with other immunosuppressive agents have not been determined. Some malignancies may be fatal. Transplant patients receiving cyclosporine are at increased risk for serious infection with fatal outcome.Serious Infections
Patients receiving immunosuppressants, including cyclosporine capsules are at increased risk of developing bacterial, viral, fungal, and protozoal infections, including opportunistic infections. These infections may lead to serious, including fatal, outcomes (see BOXED WARNING, and ADVERSE REACTIONS).Polyoma Virus Infections
Patients receiving immunosuppressants, including cyclosporine capsules, are at increased risk for opportunistic infections, including polyoma virus infections. Polyoma virus infections in transplant patients may have serious, and sometimes, fatal outcomes. These include cases of JC virus-associated progressive multifocal leukoencephalopathy (PML), and polyoma virus-associated nephropathy (PVAN), especially due to BK virus infection, which have been observed in patients receiving cyclosporine.PVAN is associated with serious outcomes, including deteriorating renal function and renal graft loss, (see ADVERSE REACTIONS, Postmarketing Experience). Patient monitoring may help detect patients at risk for PVAN.
Cases of PML have been reported in patients treated with cyclosporine capsules. PML, which is sometimes fatal, commonly presents with hemiparesis, apathy, confusion, cognitive deficiencies and ataxia. Risk factors for PML include treatment with immunosuppressant therapies and impairment of immune function. In immunosuppressed patients, physicians should consider PML in the differential diagnosis in patients reporting neurological symptoms and consultation with a neurologist should be considered as clinically indicated.
Consideration should be given to reducing the total immunosuppression in transplant patients who develop PML or PVAN. However, reduced immunosuppression may place the graft at risk.
Neurotoxicity
There have been reports of convulsions in adult and pediatric patients receiving cyclosporine, particularly in combination with high-dose methylprednisolone.Encephalopathy, including Posterior Reversible Encephalopathy Syndrome (PRES), has been described both in postmarketing reports and in the literature. Manifestations include impaired consciousness, convulsions, visual disturbances (including blindness), loss of motor function, movement disorders and psychiatric disturbances. In many cases, changes in the white matter have been detected using imaging techniques and pathologic specimens. Predisposing factors such as hypertension, hypomagnesemia, hypocholesterolemia, high-dose corticosteroids, high cyclosporine blood concentrations, and graft-versus-host disease have been noted in many but not all of the reported cases. The changes in most cases have been reversible upon discontinuation of cyclosporine, and in some cases, improvement was noted after reduction of dose. It appears that patients receiving liver transplant are more susceptible to encephalopathy than those receiving kidney transplant. Another rare manifestation of cyclosporine-induced neurotoxicity is optic disc edema including papilloedema, with possible visual impairment, secondary to benign intracranial hypertension.
Specific Excipients
Alcohol (methanol)
The alcohol content (see DESCRIPTION) of cyclosporine capsules should be taken into account when given to patients in whom alcohol intake should be avoided or minimized, e.g. pregnant or breastfeeding women, in patients presenting with liver disease or epilepsy, in alcoholic patients, or pediatric patients. For an adult weighing 70 kg, the maximum daily oral dose would deliver about 1 gram of alcohol. (See DESCRIPTIONfor alcohol content of each formulation).Care should be taken in using cyclosporine capsules with nephrotoxic drugs (see PRECAUTIONS).
Conversion from Neoral to Cyclosporine capsules
Because cyclosporine capsules (NON-MODIFIED), is not bioequivalent to Neoral ®*, conversion from Neoral ®* to cyclosporine capsules, (NON-MODIFIED) using a 1:1 ratio (mg/kg/day) may result in a lower cyclosporine blood concentration. Conversion from Neoral ®* to cyclosporine capsules, (NON-MODIFIED) should be made with increased blood concentration monitoring to avoid the potential of underdosing. -
PRECAUTIONS
General
Patients with malabsorption may have difficulty in achieving therapeutic concentrations with cyclosporine capsules.
Hypertension
Hypertension is a common side effect of cyclosporine capsules therapy (see ADVERSE REACTIONS). Mild or moderate hypertension is more frequently encountered than severe hypertension and the incidence decreases over time. Antihypertensive therapy may be required. Control of blood pressure can be accomplished with any of the common antihypertensive agents. However, since cyclosporine may cause hyperkalemia, potassium-sparing diuretics should not be used. While calcium antagonists can be effective agents in treating cyclosporine-associated hypertension, care should be taken since interference with cyclosporine metabolism may require a dosage adjustment (see Drug Interactions).
Vaccination
During treatment with cyclosporine capsules, (NON-MODIFIED), vaccination may be less effective and the use of live attenuated vaccines should be avoided.
Information for Patients
Patients should be advised that any change of cyclosporine formulation should be made cautiously and only under physician supervision because it may result in the need for a change in dosage.
Patients should be informed of the necessity of repeated laboratory tests while they are receiving the drug. They should be given careful dosage instructions, advised of the potential risks during pregnancy, and informed of the increased risk of neoplasia.
Cyclosporine may impact the ability to drive and use machines. Patients should be advised to exercise care when driving or using machines if they experience neurological disturbances including confusion, somnolence, or dizziness and discuss with their healthcare provider (see WARNINGS and ADVERSE REACTIONS).
Laboratory Tests
Renal and liver functions should be assessed repeatedly by measurement of BUN, serum creatinine, serum bilirubin, and liver enzymes.
Drug Interactions
A. Effect of Drugs and Other Agents on Cyclosporine Pharmacokinetics and/or Safety
All of the individual drugs cited below are well substantiated to interact with cyclosporine. In addition, concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) with cyclosporine, particularly in the setting of dehydration, may potentiate renal dysfunction. Caution should be exercised when using other drugs which are known to impair renal function (see WARNINGS, Nephrotoxicity).Drugs That May Potentiate Renal Dysfunction
Antibiotics Antineoplastic Antifungals Anti-Inflammatory Drugs Gastrointestinal Agents Immuno-suppressives Other Drugs ciprofloxacin
melphalan
amphotericin B
azapropazone
cimetidine
tacrolimus
fibric acid derivatives (e.g., bezafibrate, fenofibrate)
gentamicin
ketoconazole
colchicine
ranitidine
tobramycin
diclofenac
trimethoprim with sulfamethoxazole
naproxen
sulindac
vancomycin
methotrexate
During the concomitant use of a drug that may exhibit additive or synergistic renal impairment potential with cyclosporine, close monitoring of renal function (in particular serum creatinine) should be performed. If a significant impairment of renal function occurs, reduction in the dosage of cyclosporine and/or coadministered drug or an alternative treatment should be considered.
Cyclosporine is extensively metabolized by CYP 3A isoenzymes, in particular CYP3A4, and is a substrate of the multidrug efflux transporter P-glycoprotein. Various agents are known to either increase or decrease plasma or whole blood concentrations of cyclosporine usually by inhibition or induction of CYP3A4 or P-glycoprotein transporter or both. Compounds that decrease cyclosporine absorption such as orlistat should be avoided. Appropriate cyclosporine capsules dosage adjustment to achieve the desired cyclosporine concentrations is essential when drugs that significantly alter cyclosporine concentrations are used concomitantly (seeDOSAGE AND ADMINISTRATION, Blood Concentration Monitoring).
1. Drugs That Increase Cyclosporine Concentrations
Calcium Channel Blockers
Antifungals
Antibiotics
Glucocorticoids
Other Drugs
diltiazem
fluconazole
azithromycin
methylprednisolone
allopurinol
nicardipine
itraconazole
clarithromycin
amiodarone
verapamil
ketoconazole
erythromycin
bromocriptine
voriconazole
quinupristin/ dalfopristin
colchicine
danazol
imatinib
metoclopramide
nefazodone
oral contraceptives
HIV Protease inhibitors
The HIV protease inhibitors (e.g., indinavir, nelfinavir, ritonavir, and saquinavir) are known to inhibit cytochrome P-450 3A and thus could potentially increase the concentrations of cyclosporine, however no formal studies of the interaction are available. Care should be exercised when these drugs are administered concomitantly.Grapefruit juice
Grapefruit and grapefruit juice affect metabolism, increasing blood concentrations of cyclosporine, thus should be avoided.2. Drugs/Dietary Supplements That DecreaseCyclosporine Concentrations
Antibiotics
Anticonvulsants
Other Drugs/ Dietary Supplements
nafcillin
carbamazepine
bosentan
St. John’s Wort
rifampin
oxcarbazepine
octreotide
phenobarbital
orlistat
phenytoin
sulfinpyrazone
terbinafine
ticlopidine
Bosentan
Co-administration of bosentan (250 to 1,000 mg every 12 hours based on tolerability) and cyclosporine (300 mg every 12 hours for 2 days then dosing to achieve a C min of 200 to 250 ng/mL) for 7 days in healthy subjects resulted in decreases in the cyclosporine mean dose-normalized AUC, C max, and trough concentration of approximately 50%, 30% and 60%, respectively, compared to when cyclosporine was given alone (see also Effect of Cyclosporine on the Pharmacokinetics and/or Safety of Other Drugs or Agents). Coadministration of cyclosporine with bosentan should be avoided.Boceprevir
Coadministration of boceprevir (800 mg three times daily for 7 days) and cyclosporine (100 mg single dose) in healthy subjects resulted in increases in the mean AUC and C max of cyclosporine approximately 2.7-fold and 2-fold, respectively, compared to when cyclosporine was given alone.Telaprevir
Coadministration of telaprevir (750 mg every 8 hours for 11 days) with cyclosporine (10 mg on Day 8) in healthy subjects resulted in increases in the mean dose-normalized AUC and C max of cyclosporine approximately 4.5-fold and 1.3-fold, respectively, compared to when cyclosporine (100 mg single dose) was given alone.St. John’s Wort
There have been reports of a serious drug interaction between cyclosporine and the herbal dietary supplement, St. John’s Wort. This interaction has been reported to produce a marked reduction in the blood concentrations of cyclosporine, resulting in subtherapeutic levels, rejection of transplanted organs, and graft loss.Rifabutin
Rifabutin is known to increase the metabolism of other drugs metabolized by the cytochrome P-450 system. The interaction between rifabutin and cyclosporine has not been studied. Care should be exercised when these two drugs are administered concomitantly.B. Effect of Cyclosporine on the Pharmacokinetics and/or Safety of Other Drugs or Agents
Cyclosporine is an inhibitor of CYP3A4 and of multiple drug efflux transporters (e.g., P-glycoprotein) and may increase plasma concentrations of comedications that are substrates of CYP3A4, P-glycoprotein, or organic anion transporter proteins.Cyclosporine may reduce the clearance of digoxin, colchicine, prednisolone, HMG-CoA reductase inhibitors (statins) and aliskiren, bosentan, dabigatran, repaglinide, NSAIDs, sirolimus, etoposide, and other drugs.
See the full prescribing information of the other drug for further information and specific recommendations. The decision on coadministration of cyclosporine with other drugs or agents should be made by the healthcare provider following the careful assessment of benefits and risks.
Digoxin
Severe digitalis toxicity has been seen within days of starting cyclosporine in several patients taking digoxin. If digoxin is used concurrently with cyclosporine, serum digoxin concentrations should be monitored.Colchicine
There are reports on the potential of cyclosporine to enhance the toxic effects of colchicine such as myopathy and neuropathy, especially in patients with renal dysfunction. Concomitant administration of cyclosporine and colchicine results in significant increases in colchicine plasma concentrations. If colchicine is used concurrently with cyclosporine, a reduction in the dosage of colchicine is recommended.Carcinogenesis, Mutagenesis, and Impairment of Fertility
Cyclosporine gave no evidence of mutagenic or teratogenic effects in appropriate test systems. Only at dose levels toxic to dams, were adverse effects seen in reproduction studies in rats (see Pregnancy).
Carcinogenicity studies were carried out in male and female rats and mice. In the 78-week mouse study, at doses of 1, 4, and 16 mg/kg/day, evidence of a statistically significant trend was found for lymphocytic lymphomas in females, and the incidence of hepatocellular carcinomas in mid-dose males significantly exceeded the control value. In the 24-month rat study, conducted at 0.5, 2, and 8 mg/kg/day, pancreatic islet cell adenomas significantly exceeded the control rate in the low-dose level. The hepatocellular carcinomas and pancreatic islet cell adenomas were not dose related.
Cyclosporine has not been found mutagenic/genotoxic in the Ames test, the V79-HGPRT Test, the micronucleus test in mice and Chinese hamsters, the chromosome-aberration tests in Chinese hamster bone marrow, the mouse dominant lethal assay, and the DNA-repair test in sperm from treated mice. A recent study analyzing sister chromatid exchange (SCE) induction by cyclosporine using human lymphocytes in vitro gave indication of a positive effect (i.e., induction of SCE), at high concentrations in this system.
In a fertility study in rats, increased perinatal mortality and impaired postnatal development of F1 pups were observed at 15 mg/kg/day (0.2 times the MRHD based on BSA). No adverse effects on fertility and reproduction were observed up to 5 mg/kg/day (0.06 times the MRHD based on BSA) in male and female rats.
An increased incidence of malignancy is a recognized complication of immunosuppression in recipients of organ transplants. The most common forms of neoplasms are non-Hodgkin’s lymphoma and carcinomas of the skin. The risk of malignancies in cyclosporine recipients is higher than in the normal, healthy population, but similar to that in patients receiving other immunosuppressive therapies. It has been reported that reduction or discontinuance of immunosuppression may cause the lesions to regress.
Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to cyclosporine, including Neoral, during pregnancy. Encourage women who are taking Neoral during pregnancy to enroll in the Transplant Pregnancy Registry International (TPRI) by calling 1-877-955-8677 or visiting https://www.transplantpregnancyregistry.org.Risk Summary
Available data from published literature, including the Transplant Pregnancy Registry International, observational cohort studies, case-controlled studies, meta-analysis, case series, and case reports, over decades of use with cyclosporine in pregnancy have not identified a drug associated risk of major birth defects, or miscarriage. Adverse maternal or fetal outcomes including hypertension, preeclampsia, preterm birth, and low birth weight are increased in patients treated with cyclosporine. However, patients receiving cyclosporine during pregnancy have underlying medical conditions and may be treated with concomitant medications that limit the interpretability of these findings (see Data).Embryo-fetal developmental (EFD) studies in rats and rabbits with cyclosporine have shown embryo-fetal toxicity at dose levels below the MRHD based on BSA.
The alcohol content of cyclosporine capsules should be taken into account when given to pregnant women (see WARNINGS, Specific Excipients).
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
Available data from the National Transplantation Pregnancy Registry (NTPR) including 622 pregnancies in renal, liver, and heart transplant recipients exposed to cyclosporine during pregnancy found that the overall rate of major birth defects, live birth rates, and miscarriage rates were comparable to the general population. Maternal and fetal adverse outcomes, including the rate of hypertension, preeclampsia, premature births, and low birth weight infants appear to be increased in transplant recipients treated with cyclosporine compared to the general population. However, these patients have underlying medical conditions that confound the above findings.Animal Data
Animal studies have shown reproductive toxicity in rats and rabbits.Three EFD studies (two oral and one intravenous) are available in rats. In two EFD studies, pregnant rats were orally administered with cyclosporine either at doses of 10, 17, 30, 100 and 300 mg/kg/day or 4, 10 and 25 mg/kg/day from gestation day (GD) 6 to 15 or from GD 7 to 17, respectively. Maternal toxicity characterized by mortality, clinical signs of toxicity and impaired body weight gain were observed at 30 mg/kg/day and above. Cyclosporine was embryo- and fetotoxic as indicated by increased embryonic mortality and reduced fetal weight together with skeletal retardations in rats at 25 mg/kg/day and above. In addition, ventricular septal defect was observed at 25 mg/kg/day in fetuses. In the first study, the oral no observed effect level (NOEL) for both dams and fetuses was 17 mg/kg/day (0.2 times the MRHD based on BSA). In the other oral study, the NOEL for dams and fetuses were 10 and 4 mg/kg/day (0.13 and 0.05 times the MRHD based on BSA), respectively. In the IV EFD study, rats were administered with 3, 6 and 12 mg/kg/day of cyclosporine from GD 7 to 17. An increase in post implantation loss was observed at 12 mg/kg/day; ventricular septal defect was observed at ≥ 6 mg/kg/day in fetuses. The IV NOEL for dams and fetus were 6 and 3 mg/kg/day (below the MRHD based on BSA), respectively after IV administration.
In rabbits, cyclosporine was orally administered at dose levels of 10, 30, 100 or 300 mg/kg/day from GD 6 to 18. At 100 mg/kg/day and above, reduction in body weight gain of dams and at 300 mg/kg/day abortions were observed. Maternal toxicity, embryo-fetotoxicity as indicated by increased pre- and postnatal mortality, reduced fetal weight together with skeletal retardations were observed at 100 mg/kg/day and above. The NOEL for dams and fetuses was 30 mg/kg/day (1 times the MRHD based on BSA).
In two published research studies, rabbits exposed to cyclosporine in utero (10 mg/kg/day subcutaneously) demonstrated reduced numbers of nephrons, renal hypertrophy, systemic hypertension and progressive renal insufficiency up to 35 weeks of age. These findings have not been demonstrated in other species and their relevance for humans is unknown.
In a peri- and postnatal development study in rats, pregnant rats were orally administered with cyclosporine (5, 15 or 45 mg/kg/day) from GD 15 until end of lactation. At 45 mg/kg/day (0.5 times the MRHD based on BSA), increased pre and postnatal mortality of offspring and reduced body weight gain of surviving pups were observed. Cyclosporine up to 15 mg/kg/day (0.2 times the MRHD based on BSA) had no effect on pregnancy, pre and postnatal development of offspring.
Nursing Mothers
Cyclosporine and its metabolites are present in human milk following oral and intravenous administration. Adverse effects on the breastfed infant have not been reported. There are no data on the effects of the drug on milk production. The alcohol content of cyclosporine capsules should be taken into account when given to lactating women (see WARNINGS, Specific Excipients). Lactating women are encouraged to avoid additional alcohol intake during treatment. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for cyclosporine and any potential adverse effects on the breastfed infant from cyclosporine or from the underlying maternal condition.
Pediatric Use
Although no adequate and well-controlled studies have been conducted in children, patients as young as 6 months of age have received the drug with no unusual adverse effects.
Geriatric Use
Clinical studies of cyclosporine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
ADVERSE REACTIONS
The principal adverse reactions of cyclosporine capsules therapy are renal dysfunction, tremor, hirsutism, hypertension, and gum hyperplasia.
Hypertension
Hypertension, which is usually mild to moderate, may occur in approximately 50% of patients following renal transplantation and in most cardiac transplant patients.Glomerular Capillary Thrombosis
Glomerular capillary thrombosis has been found in patients treated with cyclosporine and may progress to graft failure. The pathologic changes resemble those seen in the hemolytic-uremic syndrome and include thrombosis of the renal microvasculature, with platelet-fibrin thrombi occluding glomerular capillaries and afferent arterioles, microangiopathic hemolytic anemia, thrombocytopenia, and decreased renal function. Similar findings have been observed when other immunosuppressives have been employed post transplantation.Hypomagnesemia
Hypomagnesemia has been reported in some, but not all, patients exhibiting convulsions while on cyclosporine therapy. Although magnesium-depletion studies in normal subjects suggest that hypomagnesemia is associated with neurologic disorders, multiple factors, including hypertension, high-dose methylprednisolone, hypocholesterolemia, and nephrotoxicity associated with high plasma concentrations of cyclosporine appear to be related to the neurological manifestations of cyclosporine toxicity.Clinical Studies
The following reactions occurred in 3% or greater of 892 patients involved in clinical trials of kidney, heart, and liver transplants:Randomized Kidney Patients All Cyclosporine capsules Patients Cyclosporine capsules
Azathioprine
Kidney
Heart
Liver
Body System/
(N=227)
(N=228)
(N=705)
(N=112)
(N=75)
Adverse Reactions
%
%
%
%
%
Genitourinary
Renal Dysfunction
32
6
25
38
37
Cardiovascular
Hypertension
26
18
13
53
27
Cramps
4
< 1
2
< 1
0
Skin
Hirsutism
21
< 1
21
28
45
Acne
6
8
2
2
1
Central Nervous System
Tremor
12
0
21
31
55
Convulsions
3
1
1
4
5
Headache
2
< 1
2
15
4
Gastrointestinal
Gum Hyperplasia
4
0
9
5
16
Diarrhea
3
< 1
3
4
8
Nausea/Vomiting
2
< 1
4
10
4
Hepatotoxicity
< 1
< 1
4
7
4
Abdominal Discomfort
< 1
0
< 1
7
0
Autonomic Nervous System
Paresthesia
3
0
1
2
1
Flushing
< 1
0
4
0
4
Hematopoietic
Leukopenia
2
19
< 1
6
0
Lymphoma
< 1
0
1
6
1
Respiratory
Sinusitis
< 1
0
4
3
7
Miscellaneous
Gynecomastia
< 1
0
< 1
4
3
The following reactions occurred in 2% or less of patients: allergic reactions, anemia, anorexia, confusion, conjunctivitis, edema, fever, brittle fingernails, gastritis, hearing loss, hiccups, hyperglycemia, muscle pain, peptic ulcer, thrombocytopenia, tinnitus.
The following reactions occurred rarely: anxiety, chest pain, constipation, depression, hair breaking, hematuria, joint pain, lethargy, mouth sores, myocardial infarction, night sweats, pancreatitis, pruritus, swallowing difficulty, tingling, upper GI bleeding, visual disturbance, weakness, weight loss.
Renal Transplant Patients in Whom Therapy Was Discontinued Randomized Patients
All Cyclosporine capsules Patients
Cyclosporine capsules
Azathioprine
(N=227)
(N=228)
(N=705)
Reason for Discontinuation
%
%
%
Renal Toxicity
5.7
0
5.4
Infection
0
0.4
0.9
Lack of Efficacy
2.6
0.9
1.4
Acute Tubular Necrosis
2.6
0
1.0
Lymphoma/Lymphoproliferative Disease
0.4
0
0.3
Hypertension
0
0
0.3
Hematological Abnormalities
0
0.4
0
Other
0
0
0.7
Cyclosporine capsules was discontinued on a temporary basis and then restarted in 18 additional patients.
Patients receiving immunosuppressive therapies, including cyclosporine and cyclosporine-containing regimens, are at increased risk of infections (viral, bacterial, fungal, and parasitic). Both generalized and localized infections can occur. Preexisting infections may also be aggravated. Fatal outcomes have been reported (see WARNINGS).
Infectious Complications in the Randomized Renal Transplant Patients - *
- Some patients also received ALG.
Cyclosporine capsules Treatment
Standard Treatment*
(N=227)
(N=228)
Complication
% of Complications
% of Complications
Septicemia
5.3
4.8
Abscesses
4.4
5.3
Systemic Fungal Infection
2.2
3.9
Local Fungal Infection
7.5
9.6
Cytomegalovirus
4.8
12.3
Other Viral Infections
15.9
18.4
Urinary Tract Infections
21.1
20.2
Wound and Skin Infections
7.0
10.1
Pneumonia
6.2
9.2
Postmarketing Experience
Hepatotoxicity
Cases of hepatotoxicity and liver injury including cholestasis, jaundice, hepatitis and liver failure; serious and/or fatal outcomes have been reported (see WARNINGS, Hepatotoxicity).Increased Risk of Infections
Cases of JC virus-associated progressive multifocal leukoencephalopathy (PML), sometimes fatal; and polyoma virus-associated nephropathy (PVAN), especially BK virus resulting in graft loss have been reported (see WARNINGS, Polyoma Virus Infection).Headache, Including Migraine
Cases of migraine have been reported. In some cases, patients have been unable to continue cyclosporine, however, the final decision on treatment discontinuation should be made by the treating physician following the careful assessment of benefits versus risks.Pain of Lower Extremities
Isolated cases of pain of lower extremities have been reported in association with cyclosporine. Pain of lower extremities has also been noted as part of Calcineurin-Inhibitor Induced Pain Syndrome (CIPS) as described in the literature. -
OVERDOSAGE
There is a minimal experience with overdosage. Because of the slow absorption of cyclosporine capsules, forced emesis and gastric lavage would be of value up to 2 hours after administration. Transient hepatotoxicity and nephrotoxicity may occur which should resolve following drug withdrawal. Oral doses of cyclosporine up to 10 g (about 150 mg/kg) have been tolerated with relatively minor clinical consequences, such as vomiting, drowsiness, headache, tachycardia, and in a few patients, moderately severe, reversible impairment of renal function. However, serious symptoms of intoxication have been reported following accidental parenteral overdosage with cyclosporine in premature neonates. General supportive measures and symptomatic treatment should be followed in all cases of overdosage. Cyclosporine capsules is not dialyzable to any great extent, nor is it cleared well by charcoal hemoperfusion. The oral LD 50 is 2,329 mg/kg in mice, 1,480 mg/kg in rats, and >1,000 mg/kg in rabbits. The intravenous (IV) LD 50 is 148 mg/kg in mice, 104 mg/kg in rats, and 46 mg/kg in rabbits.
-
DOSAGE AND ADMINISTRATION
Cyclosporine capsules, (NON-MODIFIED)
Cyclosporine capsules, (NON-MODIFIED) have decreased bioavailability in comparison to Neoral ®* (cyclosporine capsules, USP) MODIFIED. Cyclosporine capsules, (NON-MODIFIED) and Neoral ®* (cyclosporine capsules, USP) MODIFIED are not bioequivalent and cannot be used interchangeably without physician supervision.
The initial oral dose of cyclosporine capsules, (NON-MODIFIED) should be given 4 to 12 hours prior to transplantation as a single dose of 15 mg/kg. Although a daily single dose of 14 to 18 mg/kg was used in most clinical trials, few centers continue to use the highest dose, most favoring the lower end of the scale. There is a trend towards use of even lower initial doses for renal transplantation in the ranges of 10 to 14 mg/kg/day. The initial single daily dose is continued postoperatively for 1 to 2 weeks and then tapered by 5% per week to a maintenance dose of 5 to 10 mg/kg/day. Some centers have successfully tapered the maintenance dose to as low as 3 mg/kg/day in selected renal transplant patients without an apparent rise in rejection rate.
See Blood Concentration Monitoring,below.
Specific Populations
Renal Impairment
Cyclosporine undergoes minimal renal elimination and its pharmacokinetics do not appear to be significantly altered in patients with end-stage renal disease who receive routine hemodialysis treatments (see CLINICAL PHARMACOLOGY). However, due to its nephrotoxic potential (see WARNINGS), careful monitoring of renal function is recommended; cyclosporine dosage should be reduced if indicated (see WARNINGS and PRECAUTIONS).Hepatic Impairment
The clearance of cyclosporine may be significantly reduced in severe liver disease patients (see CLINICAL PHARMACOLOGY). Dose reduction may be necessary in patients with severe liver impairment to maintain blood concentrations within the recommended target range (see WARNINGS and PRECAUTIONS).Pediatrics
In pediatric usage, the same dose and dosing regimen may be used as in adults although in several studies, children have required and tolerated higher doses than those used in adults.Adjunct therapy with adrenal corticosteroids is recommended. Different tapering dosage schedules of prednisone appear to achieve similar results. A dosage schedule based on the patient’s weight started with 2 mg/kg/day for the first 4 days tapered to 1.0 mg/kg/day by 1 week, 0.6 mg/kg/day by 2 weeks, 0.3 mg/kg/day by 1 month, and 0.15 mg/kg/day by 2 months and thereafter as a maintenance dose. Another center started with an initial dose of 200 mg tapered by 40 mg/day until reaching 20 mg/day. After 2 months at this dose, a further reduction to 10 mg/day was made. Adjustments in dosage of prednisone must be made according to the clinical situation.
Blood Concentration Monitoring
Several study centers have found blood concentration monitoring of cyclosporine useful in patient management. While no fixed relationships have yet been established, in one series of 375 consecutive cadaveric renal transplant recipients, dosage was adjusted to achieve specific whole blood 24-hour trough concentrations of 100 to 200 ng/mL as determined by high-pressure liquid chromatography (HPLC).
Of major importance to blood concentration analysis is the type of assay used. The above concentrations are specific to the parent cyclosporine molecule and correlate directly to the new monoclonal specific radioimmunoassays (mRIA-sp). Nonspecific assays are also available which detect the parent compound molecule and various of its metabolites. Older studies often cited concentrations using a nonspecific assay which were roughly twice those of specific assays. Assay results are not interchangeable and their use should be guided by their approved labeling. If plasma specimens are employed, concentrations will vary with the temperature at the time of separation from whole blood. Plasma concentrations may range from 1/2 to 1/5 of whole blood concentrations. Refer to individual assay labeling for complete instructions. In addition, Transplantation Proceedings(June 1990) contains position papers and a broad consensus generated at the Cyclosporine-Therapeutic Drug Monitoring conference that year. Blood concentration monitoring is not a replacement for renal function monitoring or tissue biopsies.
-
HOW SUPPLIED
Cyclosporine capsules, USP (NON-MODIFIED)
25 mg
Pale reddish brown opaque body, pale reddish brown opaque cap, hard gelatin capsule, imprinted "APO" over "133" and "25" in black ink; supplied in unit dose packages of 30 (5 × 6) NDC 68084-879-25.100 mg
Reddish brown opaque body, reddish brown opaque cap, hard gelatin capsule, imprinted "APO" over "134" and "100" in black ink; supplied in unit dose packages of 30 (5 x 6) NDC 68084-921-25.Store and Dispense
Store at 20°C to 25°C (66°F to 77°F); excursions permitted from 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].FOR YOUR PROTECTION: Do not use if blister is torn or broken.
*Neoral ® (cyclosporine capsules, USP) MODIFIED manufactured by Novartis.
-
PACKAGING INFORMATION
American Health Packaging unit dose blisters (see How Supplied section) contain drug product from Apotex Corp. as follows:
(25 mg / 30 UD) NDC 68084-879-25 packaged from NDC 60505-0133
(100 mg / 30 UD) NDC 68084-921-25 packaged from NDC 60505-0134Distributed by:
American Health Packaging
Columbus, OH 432178287925/0424F
-
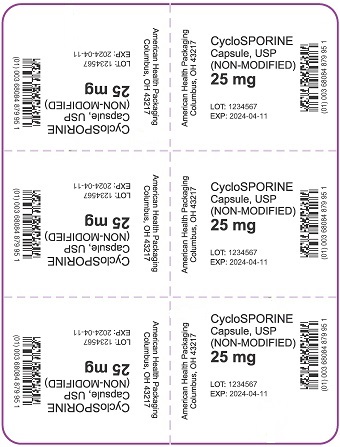
Package/Label Display Panel – Carton – 25 mg
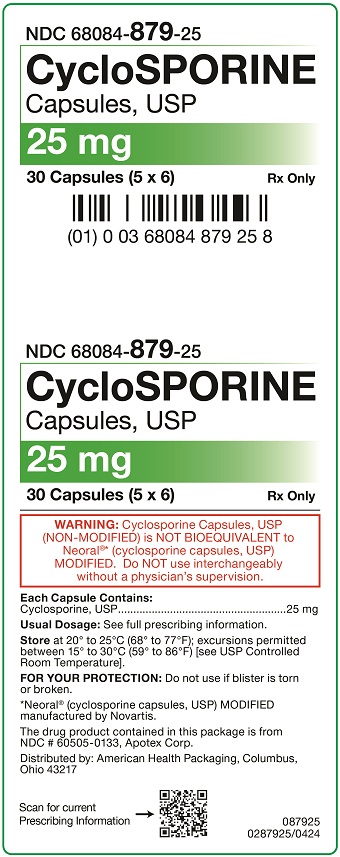
NDC 68084- 879-25
CycloSPORINE
Capsules, USP25 mg
30 Capsules (5 x 6) Rx Only
WARNING: Cyclosporine Capsules, USP
(NON-MODIFIED) is NOT BIOEQUIVALENT to
Neoral ®* (cyclosporine capsules, USP)
MODIFIED. Do NOT use interchangeably
without a physician’s supervision.Each Capsule Contains:
Cyclosporine, USP.................................................. 25 mgUsual Dosage: See full prescribing information.
Store at 20° to 25°C (68° to 77°F); excursions permitted
between 15° to 30°C (59° to 86°F) [see USP Controlled
Room Temperature].FOR YOUR PROTECTION: Do not use if blister is torn
or broken.*Neoral ® (cyclosporine capsules, USP) MODIFIED
manufactured by Novartis.The drug product contained in this package is from
NDC # 60505-0133, Apotex Corp.Distributed by: American Health Packaging, Columbus,
Ohio 43217087925
0287925/0424 - Package/Label Display Panel – Blister – 25 mg
-
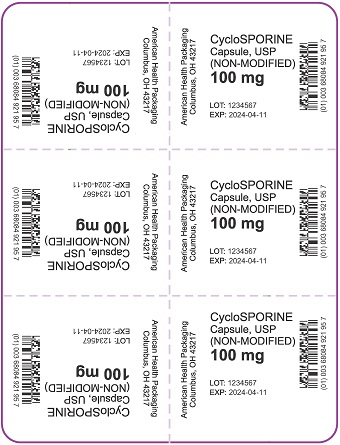
Package/Label Display Panel – Carton – 100 mg
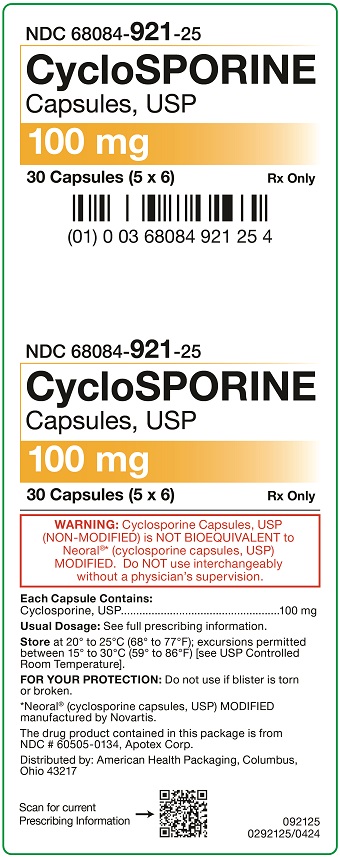
NDC 68084- 921-25
CycloSPORINE
Capsules, USP100 mg
30 Capsules (5 x 6) Rx Only
WARNING: Cyclosporine Capsules, USP
(NON-MODIFIED) is NOT BIOEQUIVALENT to
Neoral ®* (cyclosporine capsules, USP)
MODIFIED. Do NOT use interchangeably
without a physician’s supervision.Each Capsule Contains:
Cyclosporine, USP..................................................100 mgUsual Dosage: See full prescribing information.
Store at 20° to 25°C (68° to 77°F); excursions permitted
between 15° to 30°C (59° to 86°F) [see USP Controlled
Room Temperature].FOR YOUR PROTECTION: Do not use if blister is torn
or broken.*Neoral ® (cyclosporine capsules, USP) MODIFIED
manufactured by Novartis.The drug product contained in this package is from
NDC # 60505-0134, Apotex Corp.Distributed by: American Health Packaging, Columbus,
Ohio 43217092125
0292125/0424 - Package/Label Display Panel – Blister – 100 mg
-
INGREDIENTS AND APPEARANCE
CYCLOSPORINE
cyclosporine capsule, gelatin coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68084-879(NDC:60505-0133) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CYCLOSPORINE (UNII: 83HN0GTJ6D) (CYCLOSPORINE - UNII:83HN0GTJ6D) CYCLOSPORINE 25 mg Inactive Ingredients Ingredient Name Strength METHYL ALCOHOL (UNII: Y4S76JWI15) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TALC (UNII: 7SEV7J4R1U) WATER (UNII: 059QF0KO0R) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) BUTYL ALCOHOL (UNII: 8PJ61P6TS3) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) FD&C RED NO. 40 (UNII: WZB9127XOA) SHELLAC (UNII: 46N107B71O) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) ALCOHOL (UNII: 3K9958V90M) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color brown Score no score Shape CAPSULE Size 14mm Flavor Imprint Code APO;133;25 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68084-879-25 30 in 1 BOX, UNIT-DOSE 09/30/2015 1 NDC:68084-879-95 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 
Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065040 09/30/2015 CYCLOSPORINE
cyclosporine capsule, gelatin coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68084-921(NDC:60505-0134) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CYCLOSPORINE (UNII: 83HN0GTJ6D) (CYCLOSPORINE - UNII:83HN0GTJ6D) CYCLOSPORINE 100 mg Inactive Ingredients Ingredient Name Strength METHYL ALCOHOL (UNII: Y4S76JWI15) SODIUM LAURYL SULFATE (UNII: 368GB5141J) TALC (UNII: 7SEV7J4R1U) WATER (UNII: 059QF0KO0R) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) BUTYL ALCOHOL (UNII: 8PJ61P6TS3) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) FD&C BLUE NO. 1 (UNII: H3R47K3TBD) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) FD&C RED NO. 40 (UNII: WZB9127XOA) SHELLAC (UNII: 46N107B71O) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) ALCOHOL (UNII: 3K9958V90M) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color brown Score no score Shape CAPSULE Size 18mm Flavor Imprint Code APO;134;100 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68084-921-25 30 in 1 BOX, UNIT-DOSE 11/03/2015 1 NDC:68084-921-95 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 
Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065040 11/03/2015 Labeler - American Health Packaging (929561009) Establishment Name Address ID/FEI Business Operations American Health Packaging 929561009 repack(68084-879, 68084-921)